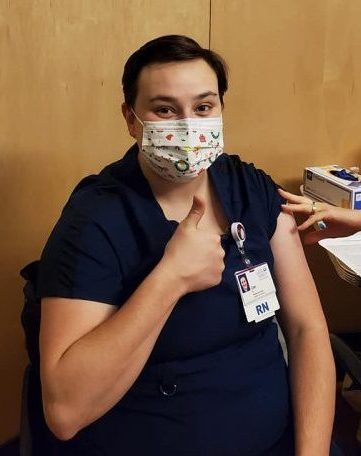
RN Zoe Melcher gets the vaccine
By CYDNEY HEED
Staff Writer
Frontline healthcare workers still face long, difficult shifts, even as the public places its faith in vaccines to end the pandemic.
Nearly a year into the pandemic, after two huge spikes that left hospitals scrambling, nurses and other frontline workers are facing burnout.
“We’re thinking maybe this is like the flu pandemic, like maybe a month or a couple weeks. Nowhere did we think it was gonna last as long as this,” said Samara Medina Vazquez, an LPN who recently earned her RN at WCC.
While healthcare jobs always have the potential to be challenging, frontline workers had to adapt quickly in the spring when the virus began to spread.
“That was definitely very intense because I had just barely gotten used to being there and I hadn’t even done a full year yet. And then suddenly we’re diving into this other kind of world where we don’t know what’s going on and every day something new was happening,” said Zoe Melcher, an RN and graduate of WCC.
While the more recent spike in cases involved fewer overall restrictions, cases were actually a lot higher than in the spring.
“The first wave that hit us we had maybe like 10 patients there that were considered positive,” said Vazquez, who works in a long-term care facility. “This second wave, though, like 87 patients in our facility of 120.”
Because of long hours and fears of passing the virus to family members, some frontline workers have also had to face separation from their loved ones.
“My kids had to go and stay with their father,” said Vazquez. “There was one of my sons already at his father’s house and I didn’t even have a chance to give him a kiss goodbye.”
All four frontline workers agreed that burnout is a concern.
“A lot of us were where we just couldn’t sleep…And then we would just literally watch a regular commercial and just immediately tears were running down their face…Because you know, you’re going through depression. Your family is separated. You’re worried about their health, but you’re not able to be close to them. But then you’re also trying to be there for these other people,” said Vazquez.
Nurses and other frontline workers have always been in high demand, but the pandemic has brought to light the extent of the shortages.
“It’s just that you know, there’s a nursing shortage in general and so when you have a sudden increase in the population that needs more than the average population, then that kind of makes it even more apparent that we need more nurses. Especially more qualified nurses that are able to take care of severely ill people, like ICU nurses,” said Melcher.
Many healthcare workers have had to take on more shifts and work longer hours in order to meet patient needs, which adds to the burnout they are experiencing.
Nurses are not the only ones who have to contend with a larger workload.
“It goes further than just nurses. A lot of people forget that there’s the housekeepers and dietary aids and the nurse assistants that are there and helping out and doing just as much work as the rest of us,” said Vazquez.
“A lot of us were working 10 [or] 14 days straight,12 to 16-hour shifts. And then you wouldn’t see them and find out they thought they had COVID. But really it was their body just shut down, like they literally just had to take a day or two,” said Vazquez.
Maintaining isolation of sick patients is a particular concern within long term care facilities, where large numbers of particularly vulnerable residents live together.
“It’s hard to keep a dementia patient still. If this patient is sick with COVID, it’s hard to say, hey, you have to stay in your room,” said Sharonda Crawley, a CNA.
One major concern that has come up since the spring is the long-term side effects of COVID-19.
“There’s definitely long-term side effects that it looks as though are irreversible,” said Lauren Demember, a tech.
Vazquez noted that the seniors in her facility who have survived COVID seem particularly affected.
“And even the residents that have survived COVID, they’re not the same…It almost progressed them into, like, further dementia,” said Vazquez.
Although healthcare workers are needed now more than ever, even they haven’t been immune to the economic effects of the pandemic. Crawley was laid off from her job in the spring when surgeries were halted.
“Because I was working OR transportation, I was contingent at the time,” said Crawley.
After that, Crawley began working in a long-term care facility.
“When I got to the nursing home, it was short-staffed, you didn’t have that many healthcare workers there. You had like almost 20 patients. The patients didn’t have family visiting. It was just sad to see,” said Crawley.
One concern among long-term care facility workers has been the emotional impact of residents not being able to visit in-person with their families. According to Vazquez, even hospice visits involved certain restrictions.
“So if your loved one was on hospice and they look like they didn’t have much longer to go, then they would set up a private room. And the family was allowed like a 30-minute visitation to pay their respects,” said Vazquez.
After two COVID-19 vaccines were given emergency approval by the FDA in December, many people have become hopeful that normalcy will return in a matter of months. Many frontline workers have already received one or both of the recommended shots.
“I got the first dose on the 30th of December…I didn’t experience really anything except fatigue one day,” said Demember.
Both Demember and Melcher experienced some side effects.
“It made me feel pretty nauseous. …And then I was very exhausted, and I kept getting headaches, and then of course pain at the site. That’s typical of any kind of…injection,” said Melcher.
However, some people, including some healthcare workers, have expressed doubts about a vaccine being created so quickly. Both Crawley and Vazquez have opted to wait a little longer before they get their shots.
Despite the challenges, Demember noted that she still loves caring for patients.
Demember said, “As hard and long as my days are, I feel like this entire period has really just reaffirmed that like nursing is definitely where I want to be. I feel very privileged to be the part of the care that these patients are getting.”


